Spatial Biology Education
The role of spatial biology in studying inflammation: A novel dimension
Posted on:
Inflammation is an essential response of our body’s immune system involving various cell types, effector molecules, and signaling pathways. However, chronic or uncontrolled inflammation can lead to various diseases, such as autoimmune disorders, sepsis, cardiovascular disorders, neurodegenerative disorders, and cancer. Thus, understanding the mechanisms and dynamics of inflammation is crucial for developing effective therapies and prevention strategies. Recently, spatial biology has emerged as a promising novel approach to study inflammation, as it enables researchers to visualize and analyze the spatial relationships between cells, tissues, and molecules within the context of the inflamed organ. By preserving the tissue integrity, researchers can identify immune cell subsets, investigate cellular interactions, and comprehend the localization of inflammatory mediators within the context of the tissue microenvironment. In this blog, we will explore the role of spatial biology in studying inflammation and highlight some of the latest findings and applications in this field.
Understanding cellular crosstalk and heterogeneity in inflammation
One of the remarkable features of inflammation is its spatial heterogeneity: different regions of the same tissue or organ can exhibit distinct cell composition and organization. Spatial biology allows researchers to dissect this spatial heterogeneity by characterizing and quantifying interactions of individual cells in distinct tissue locations. When inflammation is dysregulated, it can lead to devastating consequences, particularly in the context of chronic autoimmune diseases such as rheumatoid arthritis (RA). Montgomery et al.1 have identified and characterized two novel myeloid subpopulations in RA patients’ joints, among which a conserved group of tissue-resident monocytic-lineage cells (TR-MC). These TR-MCs have been found to possess unique cell surface markers, transcriptional programs, and thus, functions that set them apart from other immune cells. Even more intriguing, these cells exhibit rapid proliferation and reverse diapedesis in response to arthrogenic stimuli. Extravascular versus intravascular tissue location and deep phenotyping of this novel cell subset were assessed by high-throughput hyperplex experiments on the COMET™ platform. This groundbreaking research significantly enhances our understanding of RA and paves the way for developing innovative therapies to disrupt the inflammatory process, thus decreasing the burden of patients suffering from chronic joint inflammation.
Spatial dynamics and inflammation
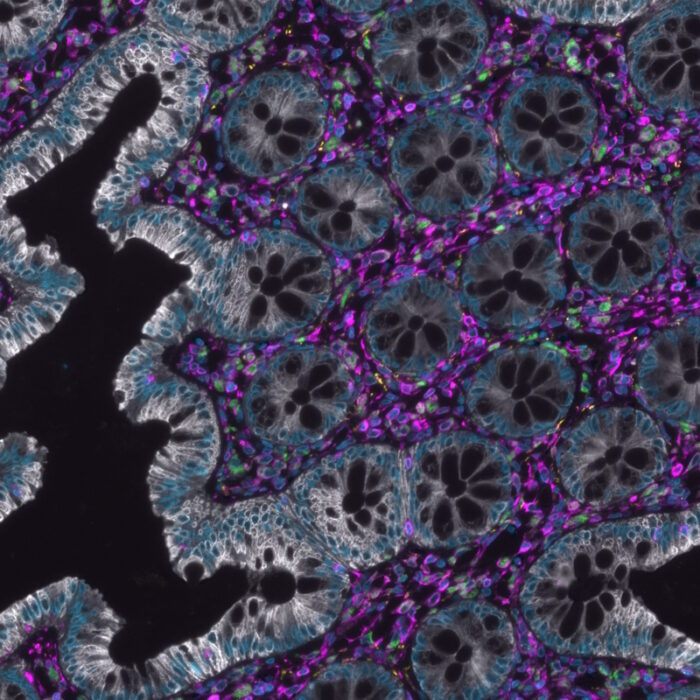
Inflammation is a dynamic process, and spatial biology can capture the dimensional changes of inflammation by monitoring the alterations in cell behavior, cytokine production, and tissue architecture over time and space. In the study by Ren et al.2, researchers found that vessel-associated macrophages (VAM) in the inflamed intestinal mucosa in mice produce a specific signaling molecule called TNF-alpha, that attracts polymorphonuclear neutrophils (PMN) to the site of inflammation. Using the hyperplex, high-throughput COMET™ platform, the authors confirmed the relevance of their findings in inflammatory bowel disease (IBD) patient biopsy specimens at the single-cell level (Figure 1). Due to the frequent correlation between the presence of PMN and tissue injury in IBD, as well as in other diseases settings, there is potential for therapeutic interventions by targeting specific macrophage populations and their disease promoting activities.2