Interview
Immuno-oncology: learn from the experts, Prof. Ascierto and Dr. Madonna
Posted on:
Immunotherapy uses the human immune system to combat diseases. In recent years, immunotherapy has transformed cancer treatment, and patients have demonstrated encouraging results in several cancer types. Regardless of the field’s potential, the number of patients that benefit from immunotherapy remains modest. As the success of immunotherapies varies greatly between patients, there is a need to investigate immune activity further and identify precise and predictive biomarkers to guide treatment options.
To mark Cancer Immunotherapy Month, we sat down with leading experts of the field, Prof. Paolo Ascierto and Dr. Gabriele Madonna, and discussed how spatial biology transforms immuno-oncology research from biomarker discoveries, the prediction of patient outcomes to the development of the next generation of personalized therapies.

Prof. Paolo Ascierto is a world-leading key opinion leader in immunotherapy. He is currently the Director of the Department of Melanoma, Cancer Immunotherapy, and Development Therapeutics at the National Cancer Institute in Naples, Italy. He is a Scientific Reviewer for leading medical journals and a Member of the Society of Melanoma Research’s Steering Committee. Dr. Ascierto is part of the Board of Directors for SITC and President of the Fondazione Melanoma Onlus & Campania Society of ImmunoTherapy of Cancer. He has presided as PI on over 150 clinical trials and is the author of more than 600 publications in peer-reviewed journals.

Dr. Gabriele Madonna is a Health Researcher at the Department of Melanoma at the National Cancer Institute in Naples. He earned his Ph.D. in Clinical and Experimental Medicine at the University of Naples, Italy. His initial research focused on the repair mechanisms for UV-induced DNA damage. Since 2010 his research interest has evolved into the study of Immunoscore and immune profiling in melanoma and the identification of potential predictive and prognostic biomarkers of response to immunotherapy and targeted therapy. He is the author of 40 peer-reviewed publications in international journals.
In immuno-oncology, there is an urgent need for sensitive tools, accurate methods, and efficient technologies. How can spatial biology support all stages of research?
Prof. Ascierto: Spatial biology allows us to study the immune contexture, which is the key to understand the immune system responsiveness and resistance to immuno-oncology therapy. In the immune contexture, the phenotype of the immune cells is vital as the functional activity and the spatial relationship between the different immune cells and tumoral cells. Spatial biology can look at all of these.
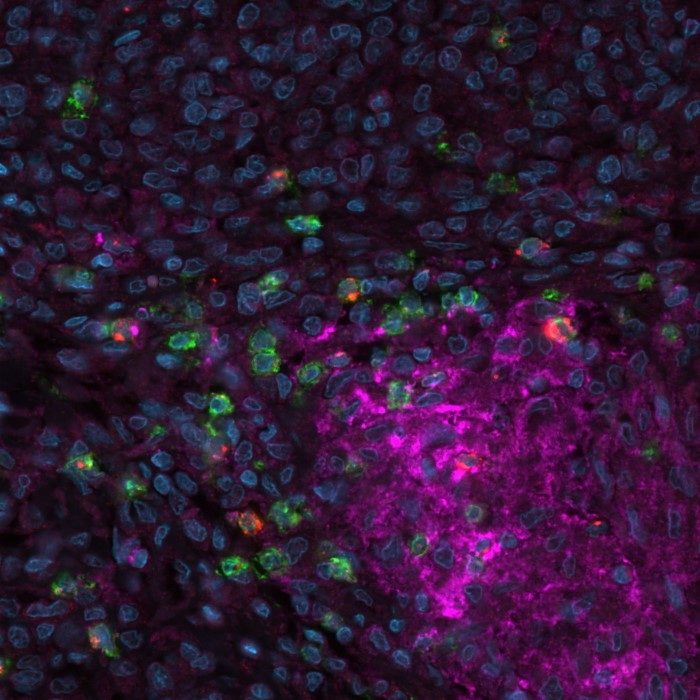
Dr. Madonna: Spatial immunofluorescence can detect dozens of biomarkers simultaneously, sometimes up to 100. We can reveal cell diversity, co-expression patterns, cellular interactions, and tissue architecture from a single tissue section. In addition, we can recognize both immune and tumor markers at the same time. By studying cells in context, we gain novel biological insights. Spatial biology span a continuum from discovery to clinical and translational research, warranting different workflows at different stages of research.
In one of your recent studies, you are analyzing the expression of PD-L1, CD8, and LAG-3 in order to stratify metastatic melanoma patients. What are other aspects of additional key immuno-oncology markers to look at?
Prof. Paolo Ascierto: In immunotherapy, we also look at tumor mutational burden (TMB) in addition to defined biomarkers. Microsatellite instability is also associated with the immunotherapy-related response, which is instrumental in the prognosis of colorectal cancer. The considerable work we did with Prof. Jérôme Galon1 was the introduction of the Immunoscore. Looking into the tumor microenvironment (TME), the Immunoscore is particularly relevant for colorectal cancer in evaluating the CD3 and CD8 at the periphery and inside the tumor.
In designing new methods to advance the field of precision immuno-oncology further, we should cover the study of different tumor parts and continue the work on identifying more precise biomarkers.
How many biomarkers should be analyzed to achieve a comprehensive patient stratification?
Prof. Paolo Ascierto: There is no rule as it depends on many factors, e.g., the biomarker, the Immunoscore, the different model system cells, and the type of cancer. The better stratification of patients and further research to advance the immuno-oncology field are critical. The goal is to create a panel of markers that can cover the most important immune system cells. Spatial biology tools are particularly valuable for identifying, visualizing, and quantifying these biomarkers.
PD-1 and LAG-3 are inhibitory immune checkpoints showing clinical benefit. Dual inhibition is being investigated in studies. Which patients could benefit the most from anti-PD-1 in combination with anti-LAG-3?
Prof. Paolo Ascierto: This is a $1 million question. LAG-3 expression was initially considered important in predicting patients’ response to therapy. However, results from the RELATIVITY-047 trial2 showed that the reality is more complicated, and LAG-3 expression alone might not be a good predictor of response. Thus, at the moment, we do not know which patients could benefit the most. Of course, this field should improve in the upcoming years.
How does spatial analysis, in particular multiplex immunofluorescence, facilitate your research?
Dr. Gabriele Madonna: Thanks to multiplex immunofluorescence, is it possible to analyze the localization and the interaction between different cells. Therefore, we prefer such an approach to genomic profiling.
Prof. Paolo Ascierto: This is the most intriguing part. For example, we know a lot about PD-L1, which might be a dynamic biomarker, but it is notably a promoter of the dynamic expression. We can look at the interaction between the different cells and the immune system with spatial biology techniques. Such information can make a difference in biomarker evaluation and is essential in distinguishing predictive and prognostic biomarkers. Soon we will be able to clearly see the importance of these interactions impacting the response to treatment.
How about the dynamic expression of biomarkers? The immune system will change during the disease. Do you believe the key biomarkers would necessarily be present before the start of the treatment?
Prof. Ascierto: This is a relevant question. However, at the moment, the baseline picture can give us more information to understand whether a patient will respond to a particular treatment or not. Before starting a treatment, it is critical to find predictive biomarkers to help doctors identify individuals who are likely to benefit from immunotherapy. From the molecular point of view, the first line and second line of treatment show other moments of the disease. In the first line, the patient did not receive treatment. Then, of course, there is a difference in the tumor microenvironment after the treatment. When starting treatment, we have to look at the TME to define the biomarkers that can predict the patient’s response.
Do you see biomarkers becoming companion diagnostics in the future?
Prof. Ascierto: If we will use the newly identified biomarkers in the context of a clinical trial and obtain positive results, why not? Surely.
What aspects of spatial immunofluorescence are relevant to accelerate the characterization of the tumor microenvironment?
Prof. Ascierto: The possibility to look not only at the phenotype but also at the functional activity of the immune system cells and the cell-to-cell interaction offered by spatial immunofluorescence is definitely at the forefront. Also, it provides the opportunity to look at the expression of subtle interactions, which are relevant for evaluating the immune context. Understanding such concepts will allow for better stratification of the patients.
Dr. Madonna: Above all, spatial biology becomes day by day faster. Spatial solutions extend the clinical benefit of immune checkpoint inhibitor therapy to appropriate patients.
How can spatial solutions and industry technology developers support the uptake of spatial biology by researchers without previous experience in spatial biology?
Prof. Ascierto: At the end of the day, spatial biology is a flexible technology that can look at several markers simultaneously. I believe that researchers will be more and more confident using spatial solutions over the years.
Dr. Madonna: During the last ten years, spatial biology has developed, starting from two/three markers. Today we are able to detect simultaneously up to 100 markers. On the other hand, not all researchers have approached these new techniques. To assist researchers in integrating spatial biology, tech companies must build open and flexible platforms to let researchers adapt their protocols, reagents, and antibodies to the new techniques.
What would be the benefits of making spatial biology mainstream among immuno-oncology researchers? How could this change the pace of discovery?
Prof. Ascierto: Spatial biology is undoubtedly the most appropriate technology in studying immune contexture. With experience and data from the most critical translational and clinical studies, it will become a must!
Dr. Madonna: Spatial biology has already driven impressive discoveries about the role of immune cells in the TME. Multiplexing is the key feature, enabling scientists to detect and analyze hundreds of proteins at the same time from the same sample.
In oncology, researchers identified signatures based on the TME. These signatures can accurately predict cancer progression or response to specific immunotherapy treatments. In the future, spatial biology will offer substantial value to clinical practice.
References:
1. Galon J. et al. Towards the introduction of the ‘Immunoscore’ in the classification of malignant tumours. J Pathol. 2014; 232(2):199-209. DOI: 10.1002/path.4287.
2. Tawbi HA. et al. Relatlimab and Nivolumab versus Nivolumab in Untreated Advanced Melanoma. Engl J Med. 2022; 386(1):24-34. DOI: 10.1056/NEJMoa2109970.

